Up until recently, cancer treatment has focused on bombarding the cancer cells with toxic chemicals or harmful radiation. This puts surrounding cells and even the entire body under stress to repair the damage caused by these stressors. But what if the body’s own natural defense system could be educated to target specific cancer cells and then enhanced and supplemented to be able to fight the cancer?
That is exactly what the new called chimeric antigen receptor (CAR) T cell therapy does. Harnessing the immune system to target cancer is the goal of this groundbreaking area of oncology research called cell therapy. Your body’s immune system normally tracks the substances that are supposed to be found in your body. If it spots a new substance that your immune system doesn’t recognize it will raise an “intruder alert” and your immune system will attack it. Unfortunately, some forms of cancer are difficult for the body to recognize and fight.
Antigens and Receptors
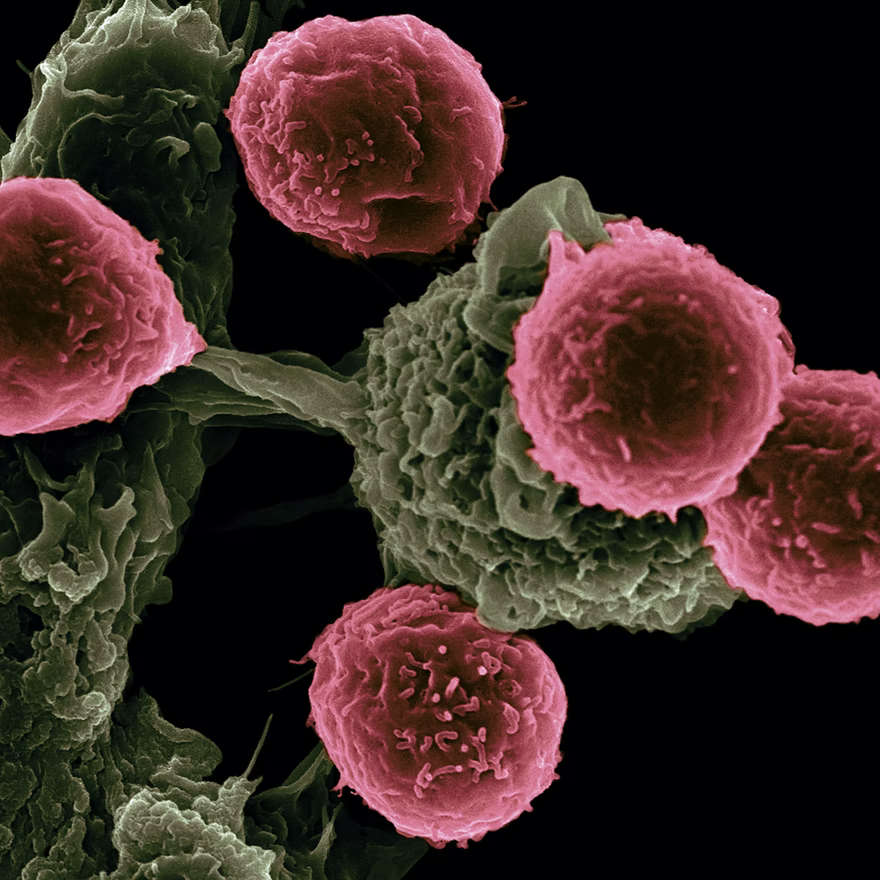
Your immune system looks for proteins called antigens on the surface of foreign cells. When they find them your immune cells have receptors called T cells that attach to foreign antigens and alert other parts of the immune system to destroy the foreign substance.
But antigens and immune receptors work like a lock and key. So you need the right immune receptor to attach to a specific antigen. Cancer cells have antigens, but if your immune cells don’t have the right receptors, they can’t attach to the antigens and help destroy the cancer cells.
CAR-T Cell Therapy
In this CAR-T Therapy, T cells are taken from a patient’s own blood and given a man-made receptor that matches the patient’s cancer cells—known as a chimeric antigen receptor (CAR). This special alteration turns the generic T cells into CAR-T cells that will attack specific cancer cells for that patient.
Then instead of the patient’s own body having to use its resources to manufacture these T cells, the T cells are grown in a lab and given to the patient by infusion.
How do researchers in the lab know it’s working?
Modern researchers are able to use a variety of instruments that actually allow them to see the T cells destroying cancer cells in real-time. Other devices use nanosensors that can detect cancer cells in the blood, which helps Doctors gauge the T cells’ progress. They also measure cytokines, which are inflammatory substances released from T cells when they’re activated.
One risk to this treatment is if the cytokine levels get too high it can cause side effects. According to the American Cancer Society:
Cytokine release syndrome (CRS): As CAR T cells multiply, they can release large amounts of chemicals called cytokines into the blood, which can ramp up the immune system. Serious side effects from this release can include:
- High fever and chills
- Trouble breathing
- Severe nausea, vomiting, and/or diarrhea
- Feeling dizzy or lightheaded
- Headaches
- Fast heartbeat
- Feeling very tired
- Muscle and/or joint pain
As doctors are gaining more experience with CAR T-cell therapy, they are learning how to recognize CRS early, as well as how to treat it.
FDA Approval
The FDA has approved CAR T-cell therapies for some kinds of lymphomas and leukemias, as well as multiple myeloma. At this point, CAR T-cell therapy is primarily used after other types of treatment have been tried. In January 2020, Janssen R&D opened a 12,000 square-foot state-of-the-art Cell Therapy Center in Pennsylvania, to further CAR-T cell research and development.
Slow Process
Currently, the process of CAR-T is complex and time-intensive—a patient has to have cells removed from their body, sent to a specialized facility where they are genetically engineered and grown, and then sent back to the patient a month later. Johnson & Johnson is hoping to speed up the process and reduce the cost by using cells from healthy donors.
Currently, CAR-T treatments are being used primarily with blood cancers like multiple myeloma, leukemia, and lymphoma, because it is easier for the t cells to migrate to the tumor sites than with solid cancers. However, research into using CAR T cells for several other types of cancer, including lymphoma, lung cancer, breast cancer, mesothelioma, ovarian cancer, and multiple myeloma is underway at Sloan Kettering Cancer Center.
Another Type of T-Cell Transfer Therapy
Another T-cell transfer therapy called tumor-infiltrating lymphocytes (or TIL) therapy is also being implemented. TIL therapy uses T cells called tumor-infiltrating lymphocytes that are found in your tumor. Doctors test these lymphocytes in the lab to find out which ones best recognize your tumor cells. Then, these selected lymphocytes are treated with substances that make them grow to large numbers quickly. So rather than genetically engineering the right lymphocytes they simply select existing ones and help them grow faster.
The idea is that these lymphocytes have already shown the ability to recognize your tumor cells. But there may not be enough of them to kill the tumor or to overcome the signals that the tumor is releasing to suppress the immune system. Giving you large numbers of the lymphocytes that react best with the tumor can help to overcome these barriers.
You might also like:
- From Pandemic To 2021 Supply Chain Disruption
- Batteries: New Sea-Water Based Battery to Replace Lithium
- Farming: Discovering New Ways to Feed the Planet
- Trends: Population, Health, and Technology
- How New Technologies Are Affecting Healthcare
- Advances in Health Technology
- Improving Your Health While Saving Money
